Photographs by Peter DiCampo
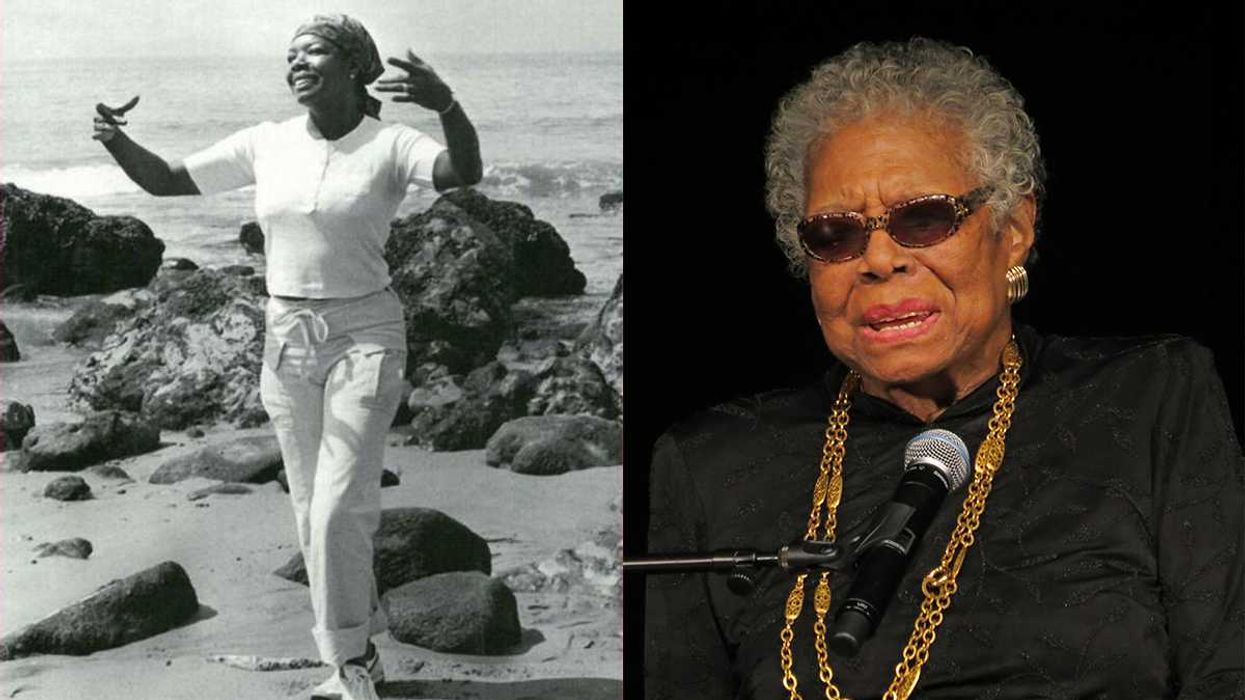
A health worker finds a young girl in Wantugu unable to walk because of an infected leg, caused by a Guinea worm that died and calcified there. Filtering dirty water is key in the Guinea worm fight, and would seem an easy solution. The fleas that feed on the worm's larvae are large-raise a glass of contaminated water to the light, and you can see them swimming around. If people pour their water through a fine mesh filter, they can keep from getting infected. "We tell people to filter their water every day," says Andrew Seidu, the head of Ghana's national Guinea worm eradication program. "But the hardest thing is getting people to change their behavior. Somewhere along the line, you will forget. Or just get fed up and stop. Or you go to visit your in-laws, and the first thing they offer you is water. Do you suddenly pull out your filter? It's the biggest disrespect."Faced with these obstacles, officials have set up multiple and overlapping methods of prevention. Foot-pedal pumps installed at ponds allow people to fill their buckets without entering the water. Guards have been hired to keep the infected out of the ponds. And local leaders have outlawed the distribution of contaminated water. Carter Center officials spend long days hunting down ponds to treat them with Abate, a chemical that kills the water fleas that consume Guinea worm larvae. Since the larvae cannot survive more than a few days without being eaten by the water fleas and then by humans, eliminating the disease from an area makes the water there safe to drink-and once the last case is cured, the larvae will cease to exist.To that end, health workers go on house-to-house rounds to make sure filters are intact and to search for active cases. Finding a victim, like Mariam Inusa, means beginning the daily process of coaxing the worm out of its human host, inch by inch.A group of small children gathers around Mariam as Dante Vasquez, a Carter Center adviser, and Faisal Hudu, his Ghanaian colleague, apply wet gauze to the open sore on the girl's knee, softening the wound and helping to loosen the worm's grip.Vasquez, a 27-year-old University of Michigan graduate with olive skin and curly brown hair, began working for the Carter Center in 2006. Hudu, also 27, was hired after volunteering with the organization at the end of college. He oversees several Savelugu neighborhoods, and Mariam is one of eight people from this area he's been treating for the month.Vasquez removes the gauze from her knee. "Has it been coming out small-small every day?" he asks, inflecting his English with some of the local patois. "It's painful small?" Mariam gives a nod. The children scramble for a better view.Vasquez pinches the worm between his left thumb and forefinger as his other hand gently massages the swollen knee. Mariam quickly places her hand over the wound. "Okay, sweetheart, small," he says softly as he moves her hand and begins to pull a bit. She wraps her fingers around his wrist. "Okay, I know it's painful. It's not going to come out otherwise." She starts to wince and wriggle. The young children laugh. Mariam tries to block Vasquez with her good knee, nearly hitting him in the face."Someone should hold her," he says, and Hudu clasps her hands as her father grabs hold from behind. She starts to writhe, pain twisting her face. She falls from the stool, struggling to free herself. She is lying on the ground now, sobbing. Vasquez is careful not to yank too hard-if the worm severs it could retreat into her knee and rot. "I don't want your worm to break, sweetheart. It will hurt even more. Trust me." She starts to scream.Health workers rest after checking the water supply in Nyujayili, Ghana. "Okay, okay," he says, and dunks the bandage in the pail and places it, wet, back on the wound. "It came out small. Some few inches," he says. Mariam sits back on the stool. Tears streak her cheeks. She keeps her left hand on the bandage.After a couple of minutes Vasquez tries again. "I just want to see," he says. But she pushes his hands away. "I won't pull. I just want to see." She lets him remove the bandage. "Can I pull small? Just a small one? Please?" Mariam is instantly thrashing and crying again. By now the young children have stopped laughing and are staring. Her father and Hudu struggle to restrain her. Another man grabs the ankle of her good leg so she can't kick anyone."I think we may be done for the day," Vasquez says. Mariam relaxes again. Hudu cleans the wound, then wraps the worm around a gauze pad, rolling it up until the pad rests snugly against her leg. It is a new take on an old method of treatment. For thousands of years people twisted their worms around small sticks, pulling a little every day. Some believe this may be the inspiration for the rod of Asclepius, the medical symbol showing a snake entwined around a staff. Hudu finishes bandaging Mariam's knee, and she wipes her eyes and glares at us as we get up to leave."That's typical," Vasquez says. "Spend several minutes. Worm comes out five or six inches. Come back the next day."
Disease eradication hasn't had a success since smallpox in 1979. Now, Guinea worm disease-in which a three-foot long worm burrows through its victim's body-is holding out in just a few African countries. The quest to wipe it out is slow and controversial, but the finish line is in sight.
Mariam Inusa sits on a low wooden stool, shivering a bit in the cool morning air. Two men crouch at the young girl's feet, next to a pail of water, and put on latex gloves. Her father stands behind her, ready to grab her arms. Mariam pulls up the printed piece of cloth that is wrapped as a skirt around her waist and legs. Emerging from a small hole in her swollen left knee is a thin white worm, six inches long, caked in blood, and dangling toward the ground.We are in Savelugu, a town of about 30,000 people in northern Ghana, 300 miles up from the country's Atlantic coast in West Africa. It is a flat town, dotted with baobab and acacia trees and bisected by a single paved road-two lanes of blacktop running north to south. Traffic is light. Sometimes a cargo truck rumbles by, but donkey carts and diesel-chugging cars and vans are more common. Mariam, tall and shy at 15 years old, lives here with her extended family in a cluster of one-story cinder-block buildings that stand around a courtyard of packed earth. Goats mill about, bleating at one another. A group of old men sit on a bench, shelling peanuts. Health workers have been visiting Mariam for about 10 days now; they have become part of the family's regular morning routine.CLICK FOR VIDEOWarning: includes scenes of a Guinea worm extraction.[good width="560" height="316" image=""]https://pre.cloudfront.goodinc.com/videos/gworms2.mp4[/good]Video by Austin MerrillThe health workers have, in fact, become a routine part of life for the entire community. The two men tending to Mariam-one Ghanaian, the other an American from Ann Arbor, Michigan-are part of an international, multi-organizational effort tasked with ridding the planet of Guinea worm, one of a handful of diseases in developing countries currently being singled-out for eradication. If they're successful, Guinea worm will be only the second disease ever to be eradicated. The first, smallpox, was wiped out nearly 30 years ago. The number of Guinea worm cases has dropped by more than 99 percent in the last 20 years, but it persists in remote parts of Africa. And as health workers fight to snuff out the last of the disease, their struggles to overcome local customs, community needs, and even dissent among global health experts demonstrate just how difficult and controversial disease eradication can be.Mariam's infection began about a year before her health-worker visits. Some time during Ghana's dry season in early 2007, she drank from a pond that was infested with a kind of water flea that feeds on Guinea worm larvae. Once humans ingest the fleas, the larvae penetrate the wall of the lower intestine and spend the next several months developing into worms. They tunnel through the body as they grow, producing an acid that ultimately forms a blister under the skin. When the victim, in an effort to relieve the burning pain, enters a pond to cool the infected area, the worm bursts through the skin, releasing millions of new larvae. The larvae are then eaten by the fleas, and the disease's life cycle continues. In most cases the worms exit from the lower legs, but they can come out anywhere-fingertips, eye sockets, breasts, genitals.Know officially as Dracunculiasis (Latin for "little dragon"), Guinea worm is an ancient ailment. Traces of the disease have been found in Egyptian mummies, and some believe it was the "fiery serpent" that plagued the Hebrews in the Bible. The pain is so acute that today it keeps children out of school and adults out of work, but since the disease is rarely fatal, it has gone through much of modern history without drawing serious attention from the global medical community. And in the same way that yellow fever and malaria fell off the priority list once they disappeared from Western countries, Guinea worm, afflicting people thousands of miles from New York or London or Geneva, was easily ignored.But Donald Hopkins, a tropical medicine specialist and alumnus of the smallpox fight, wanted to change all that. He was used to long odds-he entered medical school at the University of Chicago in 1962 as the only black student in his class after growing up in Jim Crow Miami. By the mid-1980s he was acting director of the U.S. Centers for Disease Control and Prevention, and he was eager to apply what he'd learned from smallpox to a new disease. In 1986 he convinced Jimmy Carter to make Guinea worm eradication a primary goal of the newly formed Carter Center, a nonprofit agency that would soon be known for mediating conflict, promoting democracy, and improving public health care in places like Haiti, Nicaragua, and Liberia. Because he was particularly interested in the world's lesser-known crises, Carter considered Guinea worm a perfect fit, and he hired Hopkins to lead the Guinea worm program. There were 3.5 million cases of the disease in the world when Carter and Hopkins joined forces; there are fewer than 10,000 today. The Carter Center has spent $260 million battling Guinea worm. The target date for its eradication is next year."That may slip a year or two, but I don't think much more than that," says Hopkins, who won a MacArthur "genius grant" in 1995 for his work against Guinea worm and is now vice president of health programs at the Carter Center. A fit and intense man who looks younger than his 66 years, Hopkins shuttles frequently between the center's headquarters in Atlanta and his home in Chicago, and travels to Africa whenever he can. "We're almost to the point of going out and handcuffing the last few cases to each of us to prevent transmission."The first country to knock out Guinea worm under the center's guidance was Pakistan in 1993. Kenya followed suit the next year, and then India in 1996. Over the next 10 years, eight more countries were added to the list, and four new ones-Ethiopia, Côte d'Ivoire, Burkina Faso, and Togo-reported no indigenous cases in 2007. Nigeria, Mali, and Niger still have a few hundred cases among them, but the last real bastions of Guinea worm are Sudan and Ghana.Savelugu is at the epicenter of Ghana's Guinea worm fight. An outbreak there in January, 2007, produced 533 of the country's 1,005 reported cases for that month-a one-year increase of 500 percent. The spike was the result of an unusually severe dry season in early 2006 that forced residents to get water from fewer ponds. Guinea worm victims entered those ponds to relieve pain or fill their buckets, resulting in high levels of contamination.Meanwhile in Tamale, a city of 300,000 people about 15 miles south of Savelugu, the municipal water system was falling apart due to poor maintenance and leadership. Tamale had piped clean water to several communities in the region. When its pumps failed and pipes broke, those who had relied on public spigots were suddenly forced to drink contaminated pond water. The disease spread, though no one would know it until many months later.When the outbreak hit, the Carter Center teamed up with Ghana's national Guinea worm eradication program and other agencies like UNICEF and the World Health Organization. "We doubled our efforts," Hopkins says. "We began warning Ghana in 2006 that already it was a standout among its three neighbors-Côte d'Ivoire, Burkina Faso, and Togo. Then it was even more isolated in 2007 when those countries reported no cases. Ghana finally started to get serious as a result of a lot of publicity and embarrassment."A health worker finds a young girl in Wantugu unable to walk because of an infected leg, caused by a Guinea worm that died and calcified there. Filtering dirty water is key in the Guinea worm fight, and would seem an easy solution. The fleas that feed on the worm's larvae are large-raise a glass of contaminated water to the light, and you can see them swimming around. If people pour their water through a fine mesh filter, they can keep from getting infected. "We tell people to filter their water every day," says Andrew Seidu, the head of Ghana's national Guinea worm eradication program. "But the hardest thing is getting people to change their behavior. Somewhere along the line, you will forget. Or just get fed up and stop. Or you go to visit your in-laws, and the first thing they offer you is water. Do you suddenly pull out your filter? It's the biggest disrespect."Faced with these obstacles, officials have set up multiple and overlapping methods of prevention. Foot-pedal pumps installed at ponds allow people to fill their buckets without entering the water. Guards have been hired to keep the infected out of the ponds. And local leaders have outlawed the distribution of contaminated water. Carter Center officials spend long days hunting down ponds to treat them with Abate, a chemical that kills the water fleas that consume Guinea worm larvae. Since the larvae cannot survive more than a few days without being eaten by the water fleas and then by humans, eliminating the disease from an area makes the water there safe to drink-and once the last case is cured, the larvae will cease to exist.To that end, health workers go on house-to-house rounds to make sure filters are intact and to search for active cases. Finding a victim, like Mariam Inusa, means beginning the daily process of coaxing the worm out of its human host, inch by inch.A group of small children gathers around Mariam as Dante Vasquez, a Carter Center adviser, and Faisal Hudu, his Ghanaian colleague, apply wet gauze to the open sore on the girl's knee, softening the wound and helping to loosen the worm's grip.Vasquez, a 27-year-old University of Michigan graduate with olive skin and curly brown hair, began working for the Carter Center in 2006. Hudu, also 27, was hired after volunteering with the organization at the end of college. He oversees several Savelugu neighborhoods, and Mariam is one of eight people from this area he's been treating for the month.Vasquez removes the gauze from her knee. "Has it been coming out small-small every day?" he asks, inflecting his English with some of the local patois. "It's painful small?" Mariam gives a nod. The children scramble for a better view.Vasquez pinches the worm between his left thumb and forefinger as his other hand gently massages the swollen knee. Mariam quickly places her hand over the wound. "Okay, sweetheart, small," he says softly as he moves her hand and begins to pull a bit. She wraps her fingers around his wrist. "Okay, I know it's painful. It's not going to come out otherwise." She starts to wince and wriggle. The young children laugh. Mariam tries to block Vasquez with her good knee, nearly hitting him in the face."Someone should hold her," he says, and Hudu clasps her hands as her father grabs hold from behind. She starts to writhe, pain twisting her face. She falls from the stool, struggling to free herself. She is lying on the ground now, sobbing. Vasquez is careful not to yank too hard-if the worm severs it could retreat into her knee and rot. "I don't want your worm to break, sweetheart. It will hurt even more. Trust me." She starts to scream.Health workers rest after checking the water supply in Nyujayili, Ghana. "Okay, okay," he says, and dunks the bandage in the pail and places it, wet, back on the wound. "It came out small. Some few inches," he says. Mariam sits back on the stool. Tears streak her cheeks. She keeps her left hand on the bandage.After a couple of minutes Vasquez tries again. "I just want to see," he says. But she pushes his hands away. "I won't pull. I just want to see." She lets him remove the bandage. "Can I pull small? Just a small one? Please?" Mariam is instantly thrashing and crying again. By now the young children have stopped laughing and are staring. Her father and Hudu struggle to restrain her. Another man grabs the ankle of her good leg so she can't kick anyone."I think we may be done for the day," Vasquez says. Mariam relaxes again. Hudu cleans the wound, then wraps the worm around a gauze pad, rolling it up until the pad rests snugly against her leg. It is a new take on an old method of treatment. For thousands of years people twisted their worms around small sticks, pulling a little every day. Some believe this may be the inspiration for the rod of Asclepius, the medical symbol showing a snake entwined around a staff. Hudu finishes bandaging Mariam's knee, and she wipes her eyes and glares at us as we get up to leave."That's typical," Vasquez says. "Spend several minutes. Worm comes out five or six inches. Come back the next day."
You go to visit your in-laws, and the first thing they offer you is water. Do you suddenly pull out your filter? It's the biggest disrespect.For all its humanitarian intentions, disease eradication is not without controversy. In the 1960s and 1970s, opponents of the campaign to wipe out the smallpox virus, which killed hundreds of millions of people in the first half of the 20th century alone, cited the billions of dollars that had been spent to knock off yellow fever, malaria, and other diseases-all in vain. Although the smallpox effort ultimately succeeded, not everyone was won over by the idea of amassing money and resources to target one illness, believing instead that improving basic health care and education services would save more lives than concentrating on one disease at a time."A focus on single diseases tends to be a burden on an otherwise fledgling primary health care system," says Stephen Gloyd, a professor of global health at the University of Washington. "We have to fix the system as it is, as opposed to creating some parallel system that will work really well for a while-until the funding ends, the nongovernmental organizations leave, and there's a bigger mess than when we started."But for Hopkins, projects such as Guinea worm eradication and overall public health are not mutually exclusive. Wiping out Guinea worm, he says, will free up resources to target other illnesses, often referred to as neglected tropical diseases, which do not garner as much attention or funding as AIDS or tuberculosis. While not always deadly, these diseases' crippling effects have a huge societal impact, and they require special attention. "You cannot eradicate a disease by folding it into a broader-based thing," Hopkins says. "You've got to target it specifically."Local health workers bandage newly-found Guinea worm patients after searching house-to-house for cases of the disease in Nyujayili.Money and a high profile do not guarantee quick success. The campaign against polio, led in part by the World Health Organization, is the best-known eradication effort since smallpox. The results have been checkered and costly. Polio was last seen in the Americas in 1994 and in Europe in 2002, but it persists in Africa, eight years after the eradication target date. The program's price tag since 1988 has been about $5 billion. An outbreak in Nigeria in 2003 demonstrated just how fragile eradication schemes can be. The number of cases worldwide recently had dipped below 500, but religious leaders in northern Nigeria abruptly banned the use of polio vaccines, claiming they were part of an anti-Islam sterility campaign funded by the West. The disease quickly spread to several polio-free countries in West Africa, and within two years the global totals had quadrupled.Health experts have tried to learn from such experiences, in part by seeking more input from locals. Still, Ghana would not be able to fight Guinea worm effectively without the influx of international resources. And despite the spirit of cooperation that has spread throughout the Savelugu area, not everyone agrees on what the priorities should be."We are racing against time," says Foster Kojo, a Ghanaian project officer with UNICEF. "But the water that the Carter Center wants to provide is only Guinea-worm free. There are other water-related diseases apart from Guinea worm that also have a seriously negative impact on children. We have to deal with them too. People are dying from diarrhea, from dysentery. It's a bigger issue than just a cloth filter. The overall water quality has to be taken care of as well."
Finding a victim means beginning the daily process of coaxing the worm out of its human host, inch by inch.It doesn't take much looking to see that the search for potable water-any water, really-is a major part of daily life in northern Ghana. Women are up before dawn, balancing five-gallon buckets on their heads as they walk back and forth between home and pond, often several miles in each direction. One day at a red light in Tamale, a boy steps in front of our car and into the shade of a tanker truck that is returning from a pond. He places his mouth over a leak in the tanker's rear exit valve and drinks for several seconds, stepping back with water dripping down his chest once the light turns green. "He'll probably get Guinea worm from that," says a Carter Center official as we pull away.A few days after watching Vasquez and Hudu treat Mariam, I return with them for a follow-up visit. The scene begins very much as it had before, with Hudu slicing off her old bandage and Vasquez soaking the wound for several minutes with wet gauze. Then Vasquez begins to pull the worm, and Mariam starts to cry."Sh, sh, sh, sh," Vasquez says softly as he pulls, flies buzzing around the open sore. Mariam's father struggles to hold her from behind and Hudu grabs her ankles. And then, a couple of tugs later, Vasquez pulls the last of the worm from her leg. "Mariam you are free," Vasquez says as her mother lets out a small cheer. Hudu smiles and congratulates her, and her father helps her back on to her stool. As Vasquez cleans the girl's knee, her family gathers around to look at the unfurled worm, nearly three feet in length.Vasquez, Hudu, and everyone else fighting Guinea worm in northern Ghana have had much to be upbeat about this year. There were only 27 cases of the disease in the Savelugu district in January 2008, a 96 percent reduction from the same month the year before. Similar reductions have appeared in subsequent months-90 percent in February, 94 percent in March.But there is little time for optimism while treating cases on a day-to-day basis. For all the recent progress, another widespread outbreak is only as far away as one torn filter or one child submerging her infected leg into a local pond.After we say goodbye to Mariam, our next patient is Samata Baba, a 4-year-old girl we had first met earlier that week. On our prior visit she had sat stoically as Vasquez and Hudu tended to her worm, which was emerging from the outer part of her right ankle. She had cried only at the very end, when the worm wouldn't come any more, and we had left her with a neat white bandage tied around her foot.Now her bandage is dirty and frayed, badly in need of changing. Samata climbs quietly onto a bench, pulls up her skirt, and there, on her other leg, is a second bandage, wrapped around her calf. Three days ago Samata had only one Guinea worm. Now she has two.














 Otis knew before they did.
Otis knew before they did.