This story has been sponsored by Kinsa, which believes that healthcare products in the home should always accomplish two things: reassure and comfort the user, and provide context and guidance about what to do next. Find out how they’re helping communities better track, treat, and stop the spread of illness through their smart thermometer here.
By now, you’ve surely encountered the story of the Zika virus—its enigmatic origins resemble nothing so much as a ghostly tale told round a campfire. In May 2015, doctors in Brazil were grappling with twin mysteries: First, a dramatic increase in the number of babies born with microcephaly, a condition resulting in reduced cranium size in newborns. Second, a localized outbreak of the Zika virus, the first time the disease was documented at scale in South America. Within months, the mosquito-borne Zika virus outbreak had gone from a few hundred cases to a few thousand. By Christmas Eve, Brazil declared a state of emergency; come January, the World Health Organization warned that Zika was ‘spreading explosively’ across the region.
It’s clear now that experts misjudged the situation. More than 28 countries have been affected as of this writing; Zika is officially a public health emergency that could see as many as four million people infected by the end of the year. Yet doctors admit there is still very little that they know about the Zika virus and how it spreads, which makes it difficult to curtail.
This all has an air of déjà vu to it, doesn’t it? The rapid escalation from outbreak to epidemic in such a short space of time bears an uncanny resemblance to Ebola in West Africa, ostensibly flaring from outbreak to widespread public health emergency with alarming speed. Though neither virus is new—Ebola has been around since the 1970s and Zika since the end of WWII—the leap to epidemic in both cases seems to have taken experts by surprise, despite the extensive public health surveillance systems in place.
Experts warn that the United States will be the next stop on the outbreak trail; indeed, several cases have already been reported. The country is already a lot more vulnerable to such tropical diseases in general than it used to be. But are we simply seeing a dramatic increase in dangerous infectious diseases—viruses that evolve to from minor eruption to full Pompeii in an uncontrollably short timespan—or are our monitoring and response systems simply not robust enough to cope with the variety and scale of multiple outbreaks?
According to Doctors Without Borders (MSF), it’s more the latter than the former. “It’s not necessarily that there are more of these diseases now,” says the MSF’s tropical medicine advisor Dr. Estrella Lasry, MD. “It’s more of an awareness issue… Globally, there is better reporting, and the response is also better so we’re more informed of outbreaks occurring.”
Surveillance is a different story. The top thinkers from nearly every relevant sector—be they public health workers, medical technicians, or politicians—agree that we need better surveillance tools and tracking methods. Yet the term ‘surveillance’ puts some people on edge, especially when it involves looking into public health records, our social behavior patterns, or keeping track of where we’re going. And putting so-called officials in charge of gathering data in parts of the developing world where political systems are more unstable and fluid isn’t as straightforward as it sounds.
But bodies like the WHO and MSF have been trying to drum out the message that public health surveillance is different from security surveillance, functioning as an important diagnostic tool that relies heavily on data gathered in the field by trained health workers, critical for monitoring outbreaks and developing appropriate responses. According to the Centers for Disease Control and Prevention (CDC), infectious disease surveillance gathers as much information as possible from hospital case reports, laboratory test results, and even statistics on births, deaths, marriages, and fetal deaths. Every piece of data is anonymized before it is collated, analyzed, and interpreted—and when the results are disseminated, their purpose is to help health professionals take a big-picture look so they can find patterns and, if necessary, determine whether there is an outbreak (and, if so, of which disease), and what the response should be.
In a perfect world, this would all be happening in real-time. Surveillance data could be immediately collated into a health map and experts would be able to quickly and accurately track and stop the spread of diseases. But that’s simpler said than done, not only because technology can be expensive to implement, but because tracking infectious diseases can be like quantifying smoke: The finer details are elusive.
In large part, that’s because, as Lasry says, “most disease symptoms present similarly at the start.” Fever, aches, nausea, and cramping are all common starting points for Zika, malaria, and the flu. So early symptoms are vastly underreported (especially where it’s difficult to access medical care), or patients stop seeking treatment when they feel better, even though they may still be active carriers for a dangerous virus.
Conducting the actual surveillance is also tricky; we need for more locally trained health professionals to be able to identify and respond to different diseases in the field, but health workers also need more money and resources in areas at greater risk for opportunistic infections (such as tropical or wetter regions, which are prone to more mosquitoes, as well as parts of the developing world where health systems aren’t as strong).
Lack of funding has been the hallmark in global outbreak response—often the support comes later, when the outbreak is reaching a zenith, and not at the initial stage when it would do the most good. “We [really] need better point-of-care diagnostic tools,” adds Lasry. “We need rapid diagnostic tests that are easy to use and are also not expensive.”
Those diagnostic tools may already be on the way. Learning from the Ebola outbreak, many governments and agencies are beefing up their surveillance and response capabilities. The WHO recently announced it was doing a full overhaul following criticism of its poor and haphazard response to Ebola, and President Obama has requested almost two million dollars to develop an effective response system to this Zika epidemic, which should inevitably help with similar outbreaks in the future.
The private sector is also rallying for solutions. Health workers in the field were effectively able to start getting the Ebola virus under control thanks to the invention of more sophisticated but easy to use rapid diagnostic tests (though we must note the rapid tests also increased the possibility for misdiagnosis in some cases). Increased funding for malaria in the past several years has also seen an exponential improvement in diagnostic and response tools in the field, which also experienced a recent marked decrease in fatal infection.
One promising innovation is Kinsa’s Smart Thermometer, a device that not only allows users to record and track temperature fluctuations on their phones (it plugs straight into the headset jack) but also lets them upload that information to the cloud, where researchers can track and analyze the data and spot potential outbreaks early.
This kind of interplay between data, technology, and medical knowledge can potentially be incredibly useful in slowing the spread of epidemics, according to the Journal of the American Medical Association (JAMA). If used widely, at a population level, Kina’s approach could provide a way of tracking, predicting, and possibly preventing the spread of contagious illnesses.
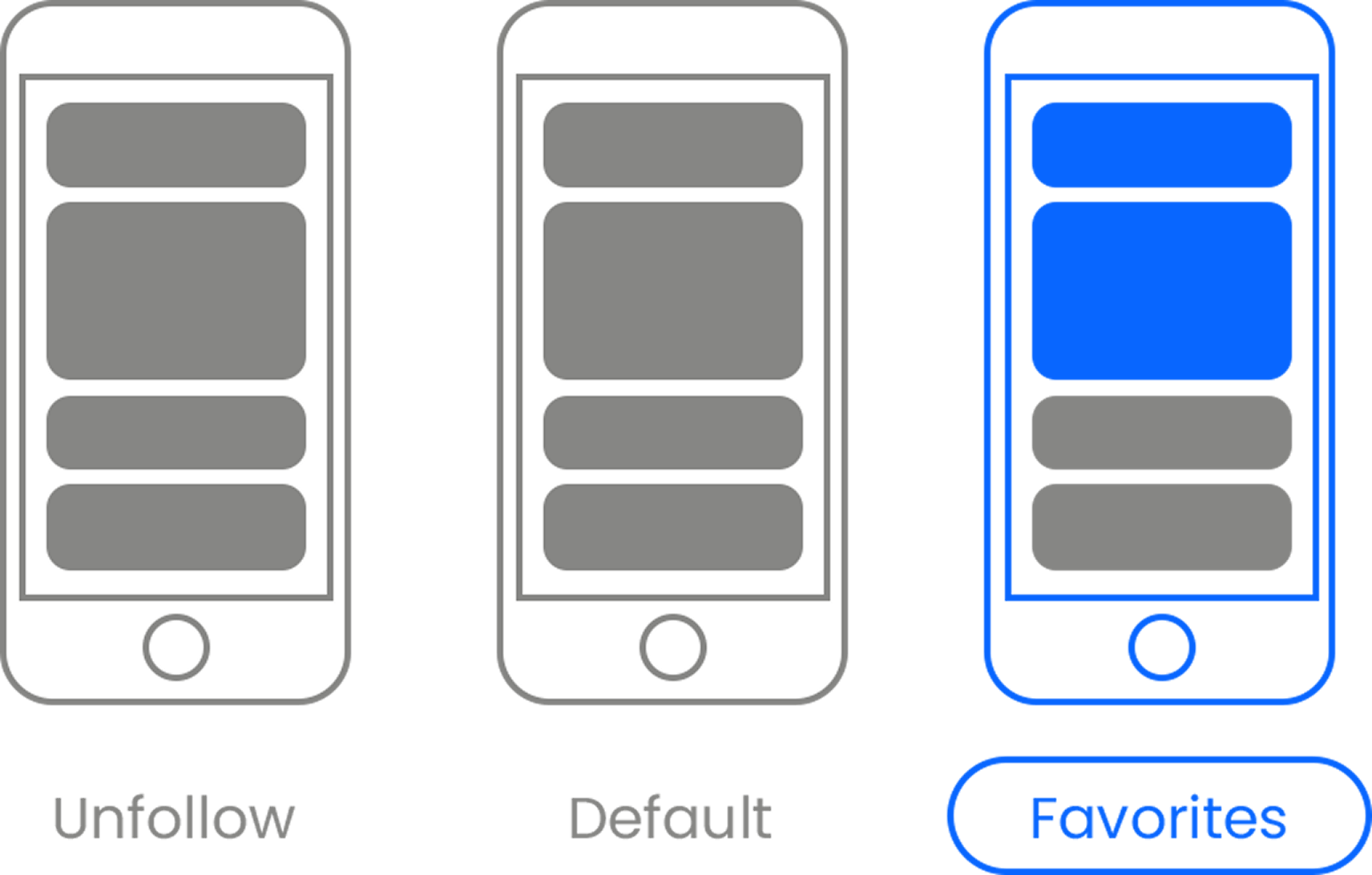
The thermometer works because “there’s a social aspect to disease,” explains Qian Qian Tang, Kinsa’s director of hardware. “Contagious diseases usually occur in pockets; they’re more concentrated than diffuse.” The proof is already in the pudding with FLUency™, Kinsa’s schools case study. By providing Smart Thermometers to children in hundreds of schools across the country, parents were able to monitor their children’s temperature spikes and share their symptoms on the phone app. This also helped parents contain the spread of contagious illnesses in two ways: First, by making diaognisis easier, as they could easily see what kinds of diseases are going around the school. And second, by knowing when to keep kids home from school.
Further down the line, Tang says that Kinsa wants to expand this functionality to fit the device into a fully integrated platform. This platform would allow the data to feed into a real-time, geo-located interactive health map that would display the locations of various outbreaks, which could potentially aid authorities as they determine where to direct their resources.
Yet these kinds of tools are just one piece of the puzzle. The rest needs to fall into place, too. “We need more [than surveillance],” says Lasry. “We also need to make sure the political will is there… Responding to outbreaks quickly [in the developing world] needs to be a bigger part of the global health and security agenda… We need to look at all the neglected diseases, not just the ones that make it out of the [developing world].”














 Otis knew before they did.
Otis knew before they did.