As time goes on, for better and for worse, artificial intelligence is making its way through several industries, including healthcare. Many insurance companies incorporate A.I. into their claims processing system with much criticism. One 2021 report quoted by CBS News found that insurers denied one out of every five claims, and it’s gotten to the point where several patients are suing their insurance providers for having A.I. determine whether or not they can afford their prescribed care. But in that wake, a new company is helping patients file their appeals with an A.I. of their own.
A major issue with using A.I. to process claims is that rejections can happen nearly instantly. This is incredibly frustrating since more health insurers aren’t allowing claims to be reviewed by flesh-and-blood doctors before accepting or rejecting them, but having their A.I. instantly review and reject them without a second opinion. When rejected, the vast majority of patients lack the medical knowledge to formally write out a successful appeal. Even if they do, the proper research could take weeks for a regular person to do and any flaw would be scrutinized by that A.I. to deny them again. That’s what caused the birth of Counterforce Health.
- YouTube youtu.be
Counterforce Health is an app that allows users to easily write up an appeal using the A.I. that the insurance companies use to process claim denials. The app allows users to upload the insurance coverage documents and the denial letter to combine them into a medically-based analytical appeal for them to print and send back to their insurance company. So far, Counterforce Health claims that 70% of the appeals it generates are accepted by the insurance company’s A.I., allowing people to get coverage for their care that was previously denied. It’s fighting fire with fire, completely free to use.
"Before you used to have a reason you would deny it, and you used to have a doctor review or a nurse review it, but once A.I. rolled out, they could just have A.I. deny it," explained Neal Shah, chairman of Counterforce Health, to ABC 11 News.
- YouTube youtu.be
Shah sees Counterforce Health as a way for people to fight back against a broken system, saying, "Sometimes when enough people get loud, enough people put pressure, then I think all of a sudden society wakes up, so I really feel like it's really about to click.”
If you don’t want to get A.I. involved or still get denied, there are still other options available to appeal again or get your claim reassessed. By law, your insurer must put in writing the reasoning why your claim is denied and provide information on how to appeal the decision through an independent third party. If you get your health insurance through your employer, your human resources representative might be able to help you or provide other resources to help fight your denial. You could also speak with your lawyer to see what litigation options are available to you. While it might not be effective and it’s not recommended, there are stories of people using social media to shame insurers into reversing their decision, too.
- YouTube youtu.be
Healthcare requires a patient to focus on healing and getting well, so depending on your circumstances it might be worthwhile to let one A.I. fight another A.I. for you.
















 Oral Wegovy pills were approved by the Food and Drug Administration in December 2025 and became available for purchase in the U.S. in January 2026.
Oral Wegovy pills were approved by the Food and Drug Administration in December 2025 and became available for purchase in the U.S. in January 2026. Despite the effectiveness of GLP-1 drugs for weight loss, there is still no replacement for healthy lifestyle patterns, including regular exercise.
Despite the effectiveness of GLP-1 drugs for weight loss, there is still no replacement for healthy lifestyle patterns, including regular exercise.

 What foods would you pick without diet culture telling you what to do?
What foods would you pick without diet culture telling you what to do?  Flexibility can help you adapt to – and enjoy – different food situations.
Flexibility can help you adapt to – and enjoy – different food situations.
 Anxious young woman in the rain.Photo credit
Anxious young woman in the rain.Photo credit  Woman takes notes.Photo credit
Woman takes notes.Photo credit 
 Revenge can feel easier than forgiveness, which often brings sadness or anxiety.
Revenge can feel easier than forgiveness, which often brings sadness or anxiety. 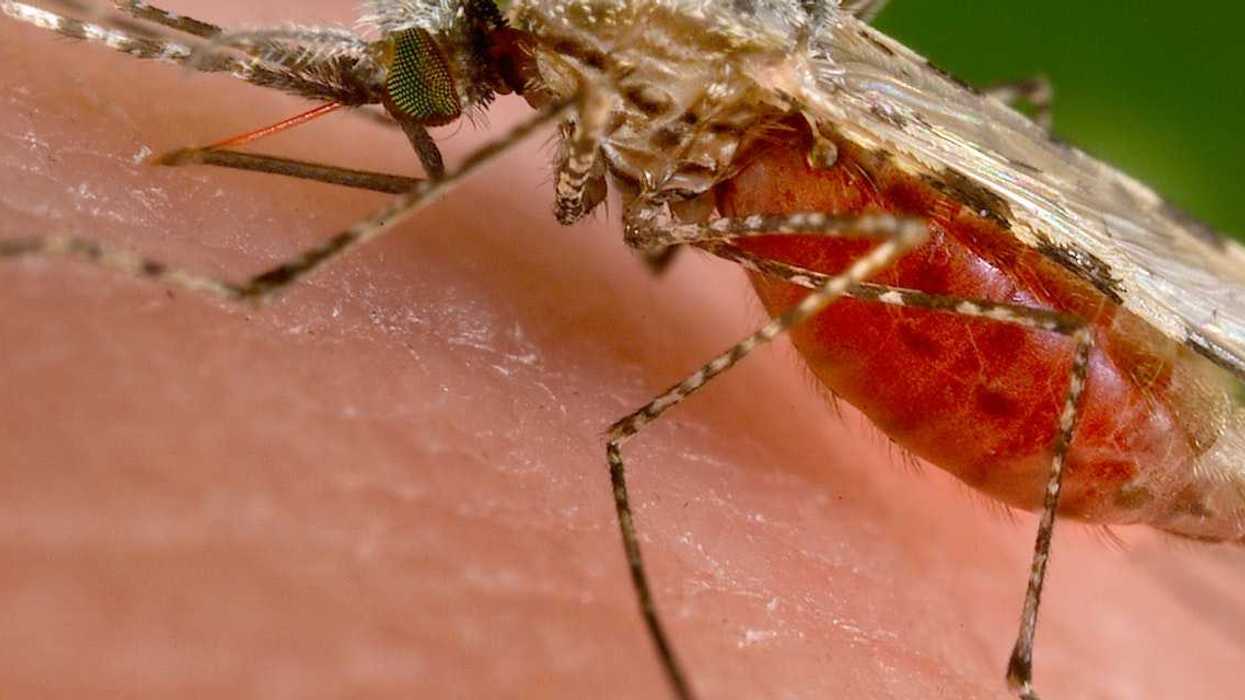
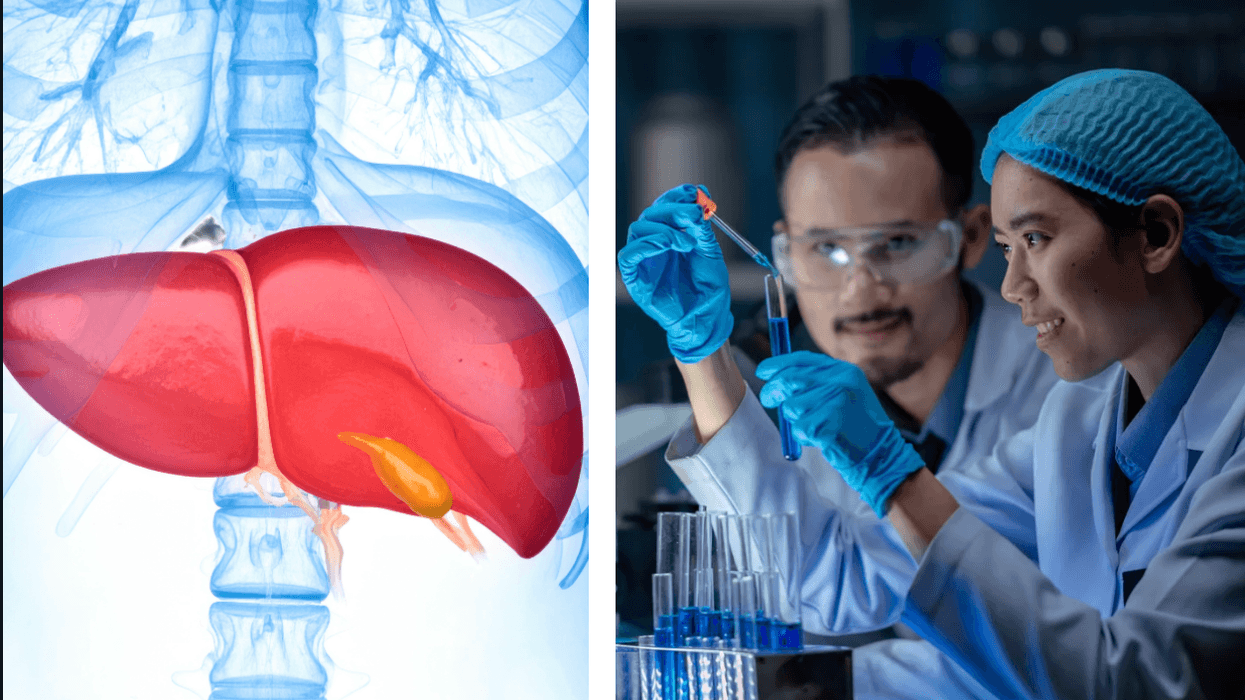
 In the past two years, two malaria vaccines have become available for babies starting at 5 months of age.
In the past two years, two malaria vaccines have become available for babies starting at 5 months of age. By exploiting vulnerabilities in the malaria parasite’s defense system, researchers hope to develop a treatment that blocks the parasite from entering cells.
By exploiting vulnerabilities in the malaria parasite’s defense system, researchers hope to develop a treatment that blocks the parasite from entering cells.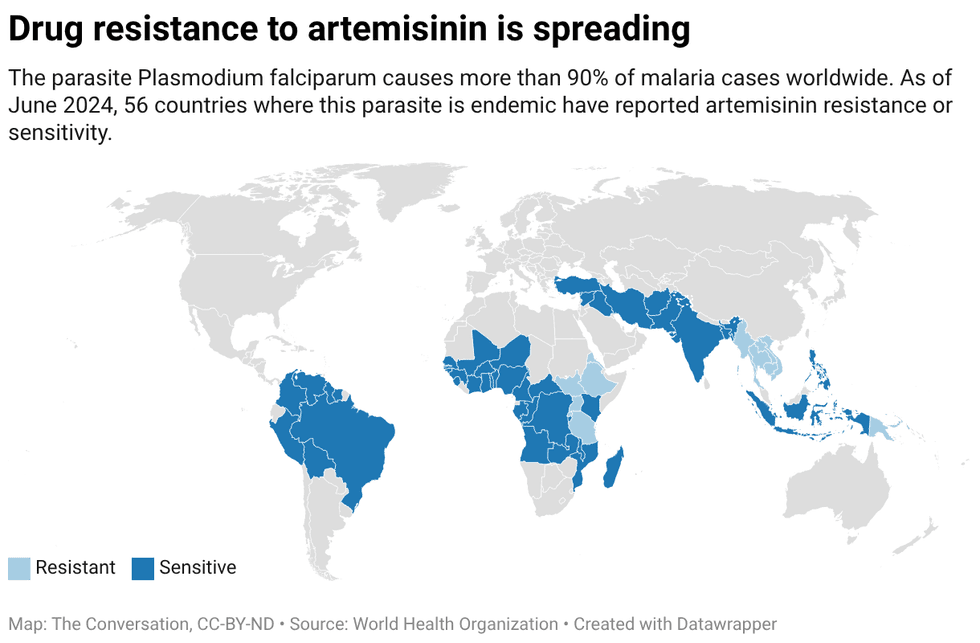 Created with
Created with