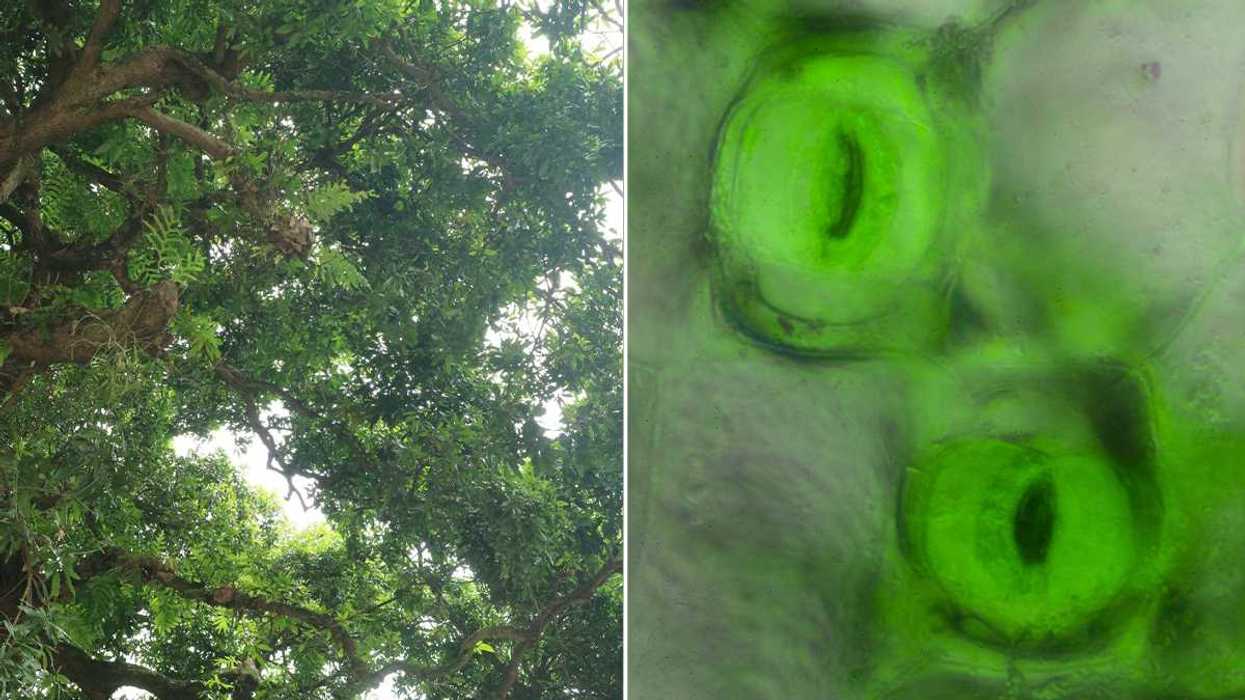
In groundbreaking news that could easily serve as the premise of a direct-to-video action movie, a Columbia University researcher has made a promising development in the fight against post-traumatic stress disorder that affects countless Americans and a disproportionate number of soldiers and veterans.
Neuroscientist Rebecca Brachman set out to address the efficacy of ketamine—a powerful psychotropic substance—as an antidepressant through experimentation with lab mice. However, since any effects of the drug wore off after a matter of hours, its utility in real-life situations seemed virtually nonexistent.
When those same subject mice were studied in another experiment to monitor how they cope with chronic stress conditions, Brachman was surprised to see that the animals treated earlier with ketamine exhibited virtually none of the depressive behavior that typically results. Subsequent reexamination and iterations of the experiment led to the same result.
It’s this subsequent depression and mental illness that plagues many PTSD sufferers, and while reactive treatment for the affliction has been the focus of much study and progress, the indication here is that this study could serve as the foundation for a new drug that could prevent the effects of PTSD before trauma is ever encountered.
Speculatively, such a drug could be administered to aid workers and soldiers in combat regions to help fight a battle against PTSD that has cost hundreds of millions of dollars per year with mixed results.
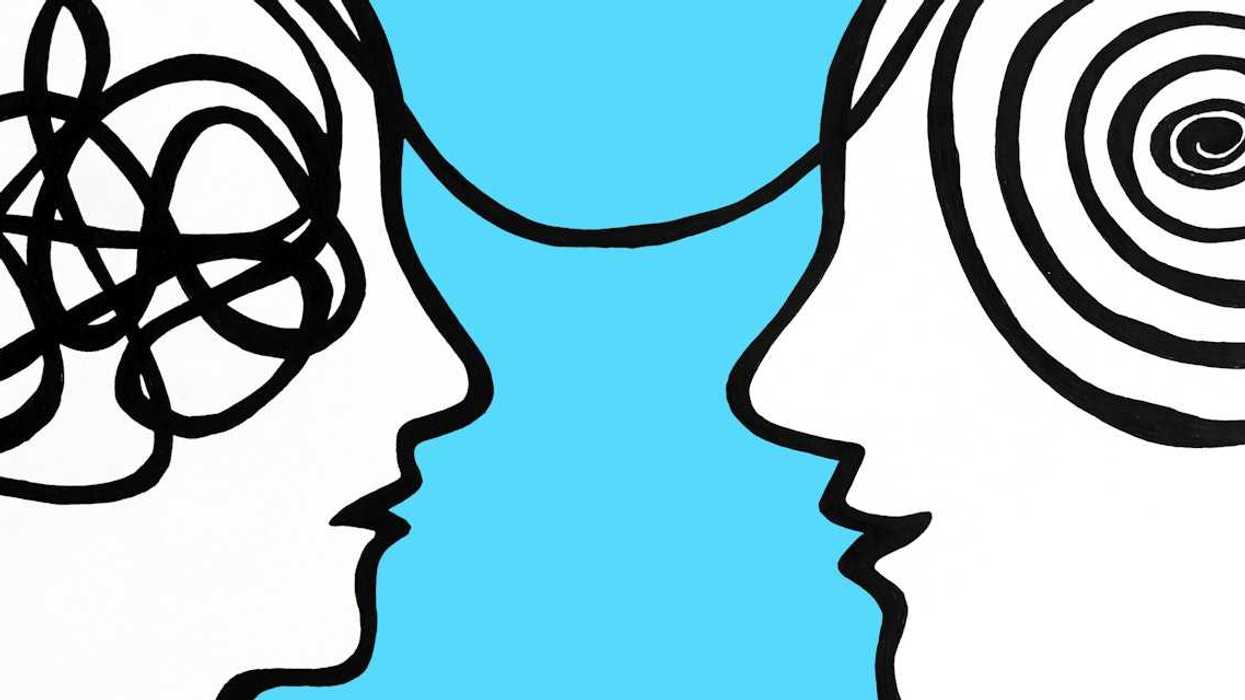
Brachman explained at a TED conference that any preemptive measures taken are further beneficial in light of the stigma surrounding mental illness and those affected:
“I think once we have treatments for diseases, or preventions for them, it really changes the conversation. Things are stigmatized in part when there’s nothing you can do about it. They’re also mythologized when there’s nothing you can do about it. From my experience, it’s more common than not. I’ve shifted my perspective from some people have mental illnesses to almost everyone I’ve ever met has had some direct experience.”
Of course, just as the drug sounds like a science-fiction-based godsend for doing good, should the developed drugs pass muster, there are equally dystopian questions surrounding the development. For instance, ketamine is a powerful synthetic drug that is used recreationally under the street name Special K, known to produce short- and long-term mental issues in those who use it.
Further, since the drug has been bandied as preventing PTSD in soldiers, it’s not hard to see a government using this to move one step closer to the “super soldier” archetype that’s prevalent in fiction. Brachman addressed this by saying she’s not seeking to “make super soldiers without empathy,” but rather offer an effective alternative to a subset of people who may be predisposed to depression or PTSD.
When viewed in a broader context of medicine, many are championing Brachman’s work here because it strives to treat mental illness in the same way other diseases are—in a proactive manner rather than in a reactive one. She spoke to this point by stating, “How quickly we get any of these treatments will depend on how as a society we prioritize it. If this is a problem that’s affecting that number of people … if other people can stand up and say ‘This is important; we have to do something,’ it gives urgency to that aspect of the conversation.”












 Regular exercise and a balanced diet are cornerstones to aging well.
Regular exercise and a balanced diet are cornerstones to aging well.


 Oral Wegovy pills were approved by the Food and Drug Administration in December 2025 and became available for purchase in the U.S. in January 2026.
Oral Wegovy pills were approved by the Food and Drug Administration in December 2025 and became available for purchase in the U.S. in January 2026. Despite the effectiveness of GLP-1 drugs for weight loss, there is still no replacement for healthy lifestyle patterns, including regular exercise.
Despite the effectiveness of GLP-1 drugs for weight loss, there is still no replacement for healthy lifestyle patterns, including regular exercise.

 What foods would you pick without diet culture telling you what to do?
What foods would you pick without diet culture telling you what to do?  Flexibility can help you adapt to – and enjoy – different food situations.
Flexibility can help you adapt to – and enjoy – different food situations.
 Anxious young woman in the rain.Photo credit
Anxious young woman in the rain.Photo credit  Woman takes notes.Photo credit
Woman takes notes.Photo credit